Factitious hyperthyroidism
 Print-Friendly
Print-Friendly
Factitious thyrotoxicosis; Thyrotoxicosis factitia; Thyrotoxicosis medicamentosa; Factitious hyperthyroxinemia
Factitious hyperthyroidism is higher-than-normal thyroid hormone levels in the blood and symptoms that suggest hyperthyroidism. It occurs from taking too much thyroid hormone medicine.
Hyperthyroidism is also known as overactive thyroid.
I Would Like to Learn About:
Causes
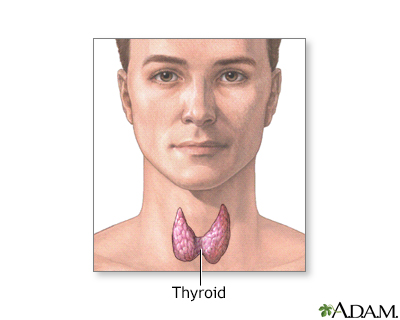
The thyroid gland produces the hormones thyroxine (T4) and triiodothyronine (T3). In most cases of hyperthyroidism, the thyroid gland itself produces too much of these hormones.
Hyperthyroidism can also be caused by taking too much thyroid hormone medicine for hypothyroidism. This is called factitious hyperthyroidism. When this occurs because the prescribed dosage of hormone medicine is too high, it is called iatrogenic, or doctor-induced, hyperthyroidism. This is common. Sometimes this is intentional (for some patients with depression or thyroid cancer), but often this happens because the dose is not adjusted based on follow up blood tests.
Factitious hyperthyroidism can also occur when someone takes too much thyroid hormone on purpose. This is very uncommon. These may be people:
- Who have mental disorders such as Munchausen syndrome
- Who are trying to lose weight
- Who are being treated for depression or infertility
Children may take thyroid hormone pills accidentally.
Symptoms
The symptoms of factitious hyperthyroidism are the same as those of hyperthyroidism caused by a thyroid gland disorder, except that:
- There is no goiter. The thyroid gland is often small.
- The eyes do not bulge, as they do in Graves disease (the most common type of hyperthyroidism).
- The skin over the shins does not thicken, as it sometimes does in people who have Graves disease.
Exams and Tests
Blood tests used to diagnose factitious hyperthyroidism include:
Other tests that may be done include radioactive iodine uptake or thyroid ultrasound.
Treatment
Your health care provider will tell you to stop taking thyroid hormone. If you need to take it, your provider will reduce the dosage.
You should be re-checked in 2 to 4 weeks to be sure that the signs and symptoms are gone. This also helps to confirm the diagnosis.
People with Munchausen syndrome will need mental health treatment and follow-up.
Outlook (Prognosis)
Factitious hyperthyroidism will resolve on its own when you stop taking or lower the dosage of thyroid hormone.
Possible Complications
When factitious hyperthyroidism lasts a long time, the same complications as untreated or poorly treated hyperthyroidism may develop:
- Abnormal heartbeat (atrial fibrillation)
- Anxiety
- Chest pain (angina)
- Heart attack
- Loss of bone mass (if severe, osteoporosis)
- Weight loss
- Infertility
- Problems sleeping
When to Contact a Medical Professional
Contact your provider if you have symptoms of hyperthyroidism.
Prevention
Thyroid hormone should be taken only by prescription and under the supervision of a provider. Regular blood tests are often needed to help your provider adjust the dose you are taking.
Related Information
| HyperthyroidismHypothyroidismPulse - bounding...Atrial fibrillatio...Chest painAnginaHeart attackOsteoporosisWeight loss - unin... | Hypothyroidism - I...Coronary artery di...Heart attack and a... |
References
Hollenberg A, Wiersinga WM. Hyperthyroid disorders. In: Melmed S, Auchus, RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 12.
Kopp P. Autonomously functioning thyroid nodules and other causes of thyrotoxicosis. In: Jameson JL, De Groot LJ, de Kretser DM, et al, eds. Endocrinology: Adult and Pediatric. 7th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 85.