Osteomyelitis
 Print-Friendly
Print-Friendly
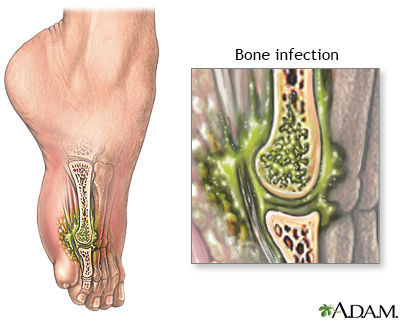
Bone infection
Osteomyelitis is a bone infection. It is caused by bacteria or other germs.
I Would Like to Learn About:
Causes
A bone infection is most often caused by bacteria. But it can also be caused by fungi or other germs. When a person has osteomyelitis:
- Bacteria or other germs may spread to a bone from infected skin, muscles, or tendons next to the bone. This may occur under a skin sore.
- The infection can start in another part of the body and spread to the bone through the blood.
- The infection can also start after bone surgery. This is more likely if the surgery is done after an injury or if metal rods or plates are placed in the bone.
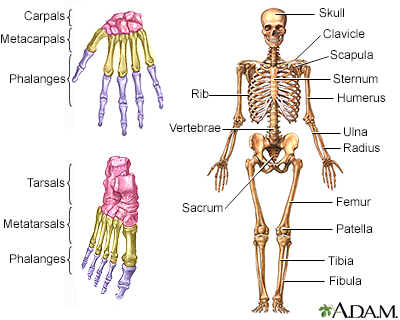
In children, the long bones of the arms or legs are most often involved. In adults, the feet, spine bones (vertebrae), and hips (pelvis) are most commonly affected.
Risk factors are:
- Diabetes
- Hemodialysis
- Poor blood supply
- Recent injury
- Use of injected illicit drugs
- Surgery involving bones
- Weakened immune system
Symptoms
Exams and Tests
Your health care provider will examine you and ask about your symptoms. The exam may show bone tenderness and possible swelling and redness in the area around the bone.
Tests may include:
- Blood culture
- Bone biopsy (the sample is cultured and examined under a microscope)
- Bone scan
- Bone x-ray
- Complete blood count (CBC) with differential
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- MRI of the bone
- Needle aspiration of the area of the affected bones
Treatment
The goal of treatment is to get rid of the infection and reduce damage to the bone and surrounding tissues.
Antibiotics are given to destroy the bacteria causing the infection:
- You may receive more than one antibiotic at a time.
- Antibiotics are taken for at least 4 to 6 weeks, often at home through an IV (intravenously, meaning through a vein).
Surgery may be needed to remove dead bone tissue if the above methods fail:
- If there are metal plates near the infection, they may need to be removed.
- The open space left by the removed bone tissue may be filled with bone graft or packing material. This promotes resolution of the infection.
Infection that occurs after joint replacement may require surgery. This is done to remove the replaced joint and infected tissue in the area. A new prosthesis may be implanted in the same operation. More often, providers wait until the antibiotic course is finished and the infection has gone away.
If you have diabetes, it will need to be well controlled. If there are problems with blood supply to the infected area, such as the foot, surgery may be needed to improve blood flow in order to get rid of the infection.
Outlook (Prognosis)
With treatment, the outcome for acute osteomyelitis is often good.
The outlook is worse for those with long-term (chronic) osteomyelitis. Symptoms may come and go for years, even with surgery. Amputation may be needed, especially in people with diabetes or poor blood circulation.
The outlook for people with an infection of a prosthesis depends partly on:
- The person's health
- The type of infection
- Whether the infected prosthesis can be safely removed
When to Contact a Medical Professional
Contact your provider if you:
- Develop symptoms of osteomyelitis
- Have osteomyelitis that continues even with treatment
Related Information
| AcuteChronicLong bonesAbscessDiabetesSubstance use | Osteomyelitis - di... | Diabetes - type 1 ... |
References
Matteson EL, Osmon DR. Infections of bursae, joints, and bones. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 251.
Raukar NP, Zink BJ. Bone and joint infections. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 125.
Tande AJ, Steckelberg JM, Osmon DR, Berbari EF. Osteomyelitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 104.