Traumatic brain injury
 Print-Friendly
Print-Friendly
Concussion; Brain injury - concussion; Traumatic brain injury - concussion; Closed head injury - concussion
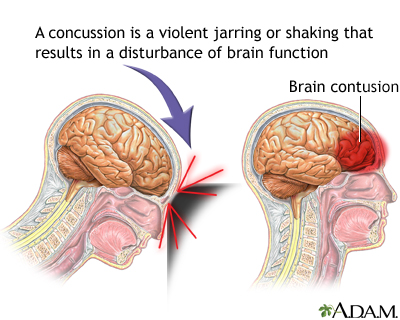
A traumatic brain injury (TBI) can occur when the head hits an object, or a moving object strikes the head. There are three types of TBI:
- Mild TBI, also called a concussion
- Moderate TBI
- Severe TBI
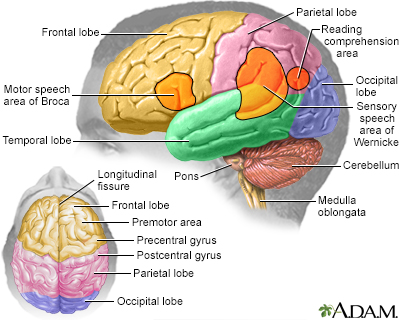
A TBI can affect how the brain works. The degree of impaired brain function and other symptoms and how long they will last depends on how severe the TBI is. A TBI may lead to headaches, changes in alertness, loss of consciousness, memory loss, and changes in thinking. Moderate to severe TBIs can cause life-long health problems.
I Would Like to Learn About:
Causes
TBIs can be caused by:
- Falls
- Sports injuries
- Vehicular accidents
- Assaults
Penetrating injuries to the skull, such as from a gunshot or other trauma can cause moderate to severe TBIs.
A big movement of the brain (called jarring) in any direction can cause a person to lose alertness (become unconscious). This movement can cause:
- The brain to bounce or twist around in the skull
- Chemical changes in the brain
- Damage to brain cells
How long the person stays unconscious may be a sign of how bad the TBI is.
Symptoms
TBI symptoms can change during recovery and are different for each person. Some symptoms may not occur right away and show up a few days or weeks later.
Symptoms of a milder TBI or concussion can include:
- Acting somewhat confused, feeling unable to concentrate, or not thinking clearly
- Being drowsy, hard to wake up, or similar changes
- Headache
- Loss of consciousness for a fairly short period of time
- Memory loss (amnesia) of events before the injury or right after
- Nausea and vomiting
- Seeing flashing lights, light sensitivity
- Feeling like you have "lost time"
- Sleep abnormalities
Mild TBIs do not always lead to loss of consciousness. Most people never pass out. They may describe seeing all white, all black, or stars. A person can also have a mild TBI and not realize it.
The following are emergency symptoms of a more severe TBI. Seek medical care right away if there are:
- Changes in alertness and consciousness
- Confusion that does not go away
- Seizures
- Muscle weakness on one or both sides of the body
- Pupils of the eyes that are not equal in size
- Symptoms in just one eye
- Unusual eye movements
- Repeated vomiting
- Walking or balance problems
- Unconsciousness for a longer period of time or that continues (coma)
Head injuries that cause a TBI often occur with injury to the neck and spine. Take special care when moving people who have had a head injury.
Exams and Tests
The health care provider will perform a physical exam. The person's nervous system will be checked. There may be changes in the person's pupil size, thinking ability, coordination, and reflexes.
Tests that may be done include:
- Blood and urine tests
- EEG (brain wave test) may be needed if seizures continue
- Head CT (computerized tomography) scan
- MRI of the brain (magnetic resonance imaging) of the brain
- X-rays
Treatment
For a mild brain injury, no treatment may be needed. But be aware that the symptoms of a brain injury can show up later.
Your providers will explain what to expect, how to manage any headaches, how to treat your other symptoms, when to return to sports, school, work, and other activities, and signs or symptoms to worry about.
- Children will need to be watched and make activity changes.
- Adults also need close observation and activity changes.
Both adults and children must follow the provider's instructions about when it will be possible to return to sports.
You will likely need to stay in the hospital if:
- Emergency or more severe symptoms of head injury are present
- There is a skull fracture
- There is any bleeding under your skull or in your brain
Outlook (Prognosis)
Healing or recovering from a TBI takes time. It may take days to weeks, or even months. During that time you may:
- Be withdrawn, easily upset, or confused, or have other mood changes
- Have a hard time with tasks that require memory or concentration
- Have mild headaches
- Be less tolerant of noise
- Be very tired
- Feel dizzy
- Have blurry vision at times
These problems will probably recover slowly. You may want to get help from family or friends for making important decisions.
In a small number of people, symptoms of the TBI do not go away. The risk for these long-term changes in the brain is higher after more than one TBI.
Seizures may occur after more severe head injuries. You or your child may need to take anti-seizure medicines for a period of time.
More severe TBIs may result in many brain and nervous system problems.
When to Contact a Medical Professional
Contact your provider if:
- A head injury causes changes in alertness.
- A person has other worrisome symptoms.
- Symptoms do not go away or are not improving after 2 or 3 weeks.
Contact your provider right away if the following symptoms occur:
- Increased sleepiness or difficulty waking up
- Stiff neck
- Changes in behavior or unusual behavior
- Changes in speech (slurred, difficult to understand, does not make sense)
- Confusion or problems thinking straight
- Double vision or blurred vision
- Fever
- Fluid or blood leaking from the nose or ears
- Headache that is getting worse, lasts a long time, or does not get better with over-the-counter pain relievers
- Problems walking or talking
- Seizures (jerking of the arms or legs without control)
- Vomiting more than 3 times
If symptoms do not go away or are not improving a lot after 2 or 3 weeks, contact your provider.
Prevention
Not all head injuries can be prevented. Increase safety for you and your child by following these steps:
- Always use safety equipment during activities that could cause a head injury. These include seat belts, bicycle or motorcycle helmets, and hard hats.
- Always use child safety seats in a car.
- Learn and follow bicycle safety recommendations.
Do not drink and drive. Do not allow yourself to be driven by someone who may have been drinking alcohol or is otherwise impaired.
Related Information
| Unconsciousness - ...Head injury - firs...ConfusionDecreased alertnes... | Concussion in adul...Concussion in chil...Concussion in chil...Concussion in adul...Preventing head in... |
References
Centers for Disease Control and Prevention website. Traumatic Brain Injury & Concussion. About mild TBI and concussion. https://www.cdc.gov/traumatic-brain-injury/about/index.html. Updated April 29, 2024. Accessed June 21, 2024.
Centers for Disease Control and Prevention website. Traumatic Brain Injury & Concussion. About moderate and severe TBI. www.cdc.gov/traumatic-brain-injury/about/moderate-severe-tbi.html. Updated January 22, 2024. Accessed June 21, 2024.
McClincy MP, Olgun ZD, Dede O. Orthopedics. In: Zitelli, BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 22.
Papa L, Goldberg SA. Head trauma. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 33.
Taylor AM, Meehan WP, Proctor MR. Sports-related traumatic brain injury (concussion). In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 729.
Trofa DP, Caldwell J-M E, Li XJ. Concussion and brain injury. In: Miller MD, Thompson SR, eds. DeLee, Drez, & Miller's Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 126.