
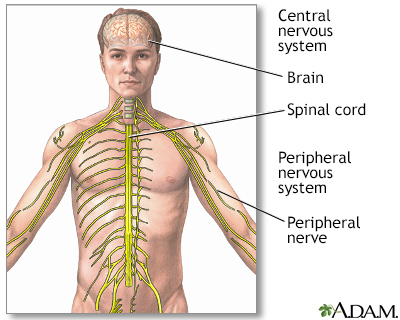
Acetylcholine receptor antibody is a protein found in the blood of many people with myasthenia gravis. The antibody affects the part of the muscle that receives signals from nerves.
This article discusses the blood test for acetylcholine receptor antibody.
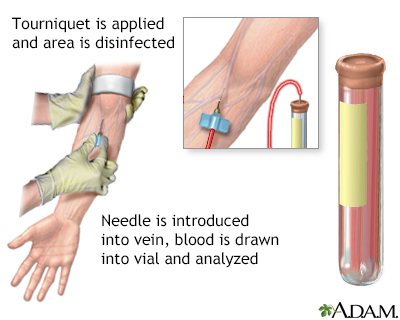

A blood sample is needed. Most of the time, blood is drawn from a vein located on the inside of the elbow or the back of the hand.
Most of the time, you do not need to take special steps before this test.
You may feel slight pain or a sting when the needle is inserted. You may also feel some throbbing at the site after the blood is drawn.
This test is used to help diagnose myasthenia gravis.
Normally, there is no acetylcholine receptor antibody (or less than 0.02 nmol/L) in the bloodstream.
Note: Normal value ranges may vary slightly among different labs. Talk to your health care provider about the meaning of your specific test results.
An abnormal result means acetylcholine receptor antibody has been found in your blood. It confirms the diagnosis of myasthenia gravis in people who have symptoms of myasthenia gravis. Nearly one half of people with myasthenia gravis that is limited to their eye muscles (ocular myasthenia gravis) have this antibody in their blood. This antibody can also be present in the blood of people who have a thymus gland tumor (thymoma), with or without myasthenia gravis.
However, the lack of this antibody does not rule out myasthenia gravis. About 1 in 5 people with myasthenia gravis do not have signs of this antibody in their blood. Your provider may also consider testing you for the muscle specific kinase (MuSK) or other antibodies.
Guptill JT, Sanders DB. Disorders of neuromuscular transmission. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 108.
Kaminski HJ. Disorders of neuromuscular transmission. In: Goldman, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 390.
BACK TO TOPReview Date: 4/16/2025
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

|
A.D.A.M., Inc. is accredited by URAC, also known as the American Accreditation HealthCare Commission (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics and subscribes to the principles of the Health on the Net Foundation (www.hon.ch). |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.